Cara couldn’t believe it. She’d gone to the bathroom only 15 minutes ago, and she was in the audience watching her daughter perform in the school play, but she had to go again. She clenched her muscles, determined not to let this thing interrupt her life, but the urgency was hard to ignore. She managed to make it until her daughter’s part was over, then ducked and hurried out of the auditorium, clenching her fists in frustration.
Cara had been to the doctor. Many times. He’d ruled out a bladder infection and found everything else to be working normally. Was this all in her head? It sure didn’t seem so. As she washed her hands and looked in the mirror, she sighed. Was this going to be her life from now on?
Fortunately for Cara and other women like her suffering from urinary frequency and urgency, what causes pelvic floor pain, and other related symptoms, there is hope. Some doctors and physical therapists have begun to diagnose women with a “new” condition known as “pelvic floor dysfunction,” with treatments looking promising..
What Is the Pelvic Floor?
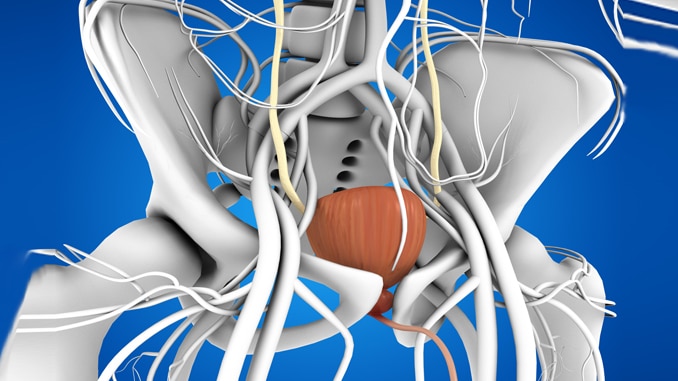
The “pelvic floor” is a group of muscles at the base of the abdomen, attached to the pelvis that supports the bladder, bowel, and uterus. They’re also called the “core” muscles. They go from front to back like a hammock, stretching from the tailbone (coccyx) to the pubic bone and side-to-side from one sitting bone to the other.
These are firm muscles that are typically strong and can move up and down as needed. Openings exist through which the urethra, which carries urine out, vagina and anus can pass through. Muscles normally wrap firmly around each of these openings to help keep them shut until they need to open. Both the anus and urethra have extra circular muscle tissues around them for firm control.
Just like you can control your arm or leg muscles, you can control your pelvic floor muscles too. That’s why you can “hold it” when you have to go to the bathroom or when you feel the need to pass gas. You contract those muscles, and they tighten around the openings. Relaxing the muscles allows urine and feces to pass through.
You use these muscles during sexual intercourse too as they control the vaginal opening. In women, squeezing can help contribute to sexual sensation and arousal. When pregnant, the muscles provide support for the fetus and assist in the birthing process. Finally, these muscles work with the abdominals and back muscles to stabilize and support the spine, and they also help when you’re lifting or exercising.
Pelvic Floor Muscles Can Become Weakened and Stretched
As women age, pelvic floor muscles can become weakened and stretched, after which they can no longer support the pelvic organs as well as they once did.
Some things that can cause these muscles to loosen include:
- Pregnancy and childbirth: Women who have had multiple births, large babies, severe perineal tearing or went through births where tools were used (forceps) are more at risk for pelvic muscle damage.
- Chronic coughing: Those with diseases that lead to chronic coughing or who smoke regularly are at risk.
- Heavy lifting: If you regularly lift heavy things, you can strain the muscles in the pelvic floor. Overzealous weight training can also cause this strain.
- High-impact exercise: In time, this can cause muscle strain in the pelvic floor.
- Age: Moreover, just like all muscles tend to weaken with age, the pelvic floor muscles do too. Regular exercises can help.
- Obesity: Extra weight puts pressure on the pelvic floor muscles and may lead to strain.
- Straining on the toilet: If you regularly strain when on the toilet — if you suffer from constipation — the muscles may weaken and loosen.
- History of back pain: Studies show that those with low back pain have a significant increase in pelvic floor dysfunction compared to those without back pain.
Muscles can become loose, but they can also become too tight. You know the feeling when you’ve been holding your shoulders too tight because of tension? You end up with shoulder pain, right?
The same thing can happen to your pelvic floor muscles. They may fail to relax properly, which can cause incomplete emptying in the bladder and bowel as well as pain during intercourse. Many women with tight pelvic floor muscles may not even realize what’s happening as the symptoms seem to mimic other issues like urinary tract infections and stress urinary incontinence.
Symptoms of a Pelvic Floor Problem
Might you be suffering from a pelvic floor issue? It’s not always easy to tell, but symptoms may include the following:
- Urinary frequency and urgency
- Accidental urine leakage when laughing, coughing or exercising
- Difficulty emptying the bladder or bowel completely
- Accidentally losing control of the bladder or bowel
- Pain in the pelvic area
- Painful intercourse
- Pelvic prolapse, which is where the pelvic muscles loosen enough to allow some of the organs to drop; women may feel a bulge in the vagina or a feeling of heaviness
The actual pelvic pain may range from mild to severe. It may feel like a dull ache or a sharp pain and may come and go or persist more constantly.
Many Possible Causes of Pelvic Floor Pain in Women
What Causes Pelvic Floor Pain: Pelvic floor pain and other related systems may be caused by a number of things. Below are the most common causes related to the female reproductive system. Sometimes, a person may have more than one condition that contributes to pelvic pain:
- Endometriosis: Tissue that lines the inside of the uterus grows outside of it, instead, which can cause pelvic pain. Adenomyosis, a related condition in which the tissue grows into the muscular wall of the uterus, can cause similar pain.
- Ectopic pregnancy: The fertilized egg grows outside the uterus. As the fetus grows, it can cause pelvic pain.
- Menstrual cramps: As most women know, the menstrual period can cause cramping pains in the lower abdomen.
- Miscarriage: When the pregnancy ends in miscarriage, there can be pain and cramping.
- Mittelschmerz: Ovulation causes pain, usually in the middle of the menstrual cycle.
- Ovarian cysts or cancer: Cysts are fluid-filled sacs that can form on the ovaries. Most are harmless, but some can cause pain, particularly on one side.
- Pelvic inflammatory disease (PID): This is an infection of a woman’s reproductive organs, and it may cause pelvic pain and abnormal bleeding.
- Uterine fibroids: These are benign (noncancerous) tumors that grow in the uterus. Most are harmless, but some can cause symptoms like pain and frequent urination.
- Vulvodynia: Chronic pain around the opening of the vagina that has no identifiable cause is called “vulvodynia.” It can cause pain during intercourse.
What Causes Pelvic Floor Pain: Pelvic floor pain isn’t always a reproductive issue, however. Sometimes, the following conditions may cause symptoms:
- Appendicitis: The appendix, which is on the lower right side of the abdomen, becomes inflamed and can cause sudden pain on that side.
- Colon cancer: The large intestine develops cancerous tumors, which can cause cramps and pain.
- Constipation: If you have fewer than three bowel movements a week, you may be suffering from constipation, which can cause straining, pain and incomplete emptying.
- Inflammatory bowel disease: These include Crohn’s disease and ulcerative colitis, both of which cause inflammation in the digestive tract. This inflammation often leads to pain.
- Diverticulitis: Small pouches form in the lining of the digestive system, which are usually harmless. Sometimes, these can cause severe abdominal pain.
- Fibromyalgia: This is a disorder that involves widespread pain, which may include pelvic pain.
- Inguinal hernia: These are hernias (bulges) that develop in the abdominal muscles and may cause pain or discomfort in the abdomen and pelvic area.
- Interstitial cystitis: Also called “painful bladder syndrome,” this condition causes bladder pressure and pain and sometimes pelvic pain.
- Intestinal obstruction: If a blockage develops in the intestines, cramps and abdominal pain may develop.
- Irritable bowel syndrome: This is a disorder that causes general discomfort in the digestive tract, including cramping and abdominal pain.
- Kidney stones: These are hard mineral deposits that form inside the kidneys and then try to move through the urethra and out of the body. If they are large, they can cause pain.
- Urinary tract infection: Microorganisms get into the urinary system and cause an infection. The infection may exist in the urethra, bladder and/or kidneys. Symptoms include urinary urgency and frequency and pelvic pain.
Sometimes, the pelvic floor muscles tighten and spasm, much like any other muscle might.
Specific Pelvic Floor Disorders
Although all of the conditions above may cause pelvic pain, that pain is related to some other issue. If the problem is with the muscles themselves, however, the issue is that the muscles have become weakened and stretched. Possible outcomes include:
- Urinary incontinence (loss of bladder control)
- Fecal incontinence (loss of bowel control)
- Pelvic organ prolapse (uterus, bladder or bowel “drop” into the vagina and cause a bulge)
What Causes Pelvic Floor Pain: Problematic pelvic floor muscles may cause any of these issues, so treatments will focus on either strengthening those muscles or providing them with additional support. Women can check with a gynecologist or urologist for help.
Furthermore, doctors are likely to suggest exercises like Kegel exercises first to help strengthen the muscles. Additionally, if symptoms persist or interfere with everyday life, minimally invasive surgery may be needed to provide extra support for the pelvic organs.
What Is Pelvic Floor Dysfunction?
Some women go through a myriad of tests and see many doctors only to be told that they are “fine.” What then?
That’s when a diagnosis of “pelvic floor dysfunction” may apply. This means that the muscles are not cooperating. There is either too much tension in the muscles, or they are too relaxed.
What Causes Pelvic Floor Pain: Symptoms are similar to other related conditions and usually include urinary frequency and urgency, pelvic pain, low back pain, bowel problems and potentially pain with intercourse. Many women have symptoms that are similar to a urinary tract infection, but tests show no evidence of an infection. If urine emptying is slow or spastic, the muscles may be too tight or locked in a spasm. If urine is difficult to control, they may be too relaxed.
What causes this condition? Doctors still aren’t sure, but they have discovered many things that can set it off:
- Traumatic childbirth that damages nerves
- Weakness or tension in the hip, back or pelvic floor
- Recurring urinary tract infections
- Past injury that causes you to put stress on other muscles
Women may struggle to get an accurate diagnosis, however, because not all doctors recognize “pelvic floor dysfunction” as a condition. Awareness is growing, however, so if you’re not getting the help you need, don’t hesitate to seek out another medical professional.
Current treatments for pelvic floor dysfunction include:
- Watchful waiting — sometimes the symptoms will go away on their own
- Lifestyle changes — working on relaxation, deep breathing and meditation since stress can contribute to symptoms
- Medications that help soothe the bladder so it will relax
- Moreover, kegel exercises to strengthen the pelvic floor muscles
- Core exercises to help strengthen the abdominal muscles
- Biofeedback to improve relaxation
- Retraining the bladder — patients work on extending the period of time between bathroom visits
- Physical therapy that helps retrain the muscles to perform as they should; this may include deep tissue massage, myofascial release and trigger point therapy
If you have low back pain too, treating the low back pain through various stretches, massage and possibly yoga may also help relieve pelvic floor pain.
If you want to strengthen your core and back, flatten your belly and achieve your dream abs while keeping yourself injury free, then check out the Invincible Core program.
References
Arab, A. M., Behbahani, R. B., Lorestani, L., & Azari, A. (2010). Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Manual Therapy, 15(3), 235-239. doi:10.1016/j.math.2009.12.005
Haran, C. (2006, January 6). New Explanation for Women’s Pelvic Pain? Retrieved from https://abcnews.go.com/Health/story?id=116735&page=1
Interstitial Cystitis Association. (n.d.). Pelvic Floor Dysfunction – Interstitial Cystitis Association. Retrieved from https://www.ichelp.org/about-ic/associated-conditions/pelvic-floor-dysfunction/
Pelvic floor muscles · The facts · Continence Foundation of Australia. (n.d.). Retrieved from https://www.continence.org.au/pages/how-do-pelvic-floor-muscles-help.html
Physiopedia. (n.d.). Low Back Pain and Pelvic Floor Disorders. Retrieved from https://www.physio-pedia.com/Low_Back_Pain_and_Pelvic_Floor_Disorders#cite_note-Three-3
Signs of a pelvic floor problem · The pelvic floor · Pelvic Floor First. (n.d.). Retrieved from https://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html