Parkinson’s disease can cause stiffness, balance issues, and muscle rigidity, but gentle stretching can provide significant relief. Incorporating specific stretches into your routine can improve flexibility, increase mobility, and reduce discomfort.
In this post, we’ll show you five safe, effective stretches designed to help those with Parkinson’s disease [1] maintain functional movement and stay pain-free.
These Parkinson’s disease exercises are easy to perform and can be done at home, offering an accessible way to enhance your quality of life while managing symptoms.
1. Chest Muscle Stretch
This stretch helps counteract the rounded posture common in PD patients.

- Sit or stand with your hands behind your head.
- Ask someone to gently pull your elbows back until you feel a stretch in the chest and armpit area.
- Hold for 15 seconds. Repeat 3 times.
Alternative: Stand in a doorway with arms out in a T-position. Lean forward to stretch the chest. Hold and repeat as above.
2. Calf Stretch with a Towel
Tight calves can impair gait and balance. This seated stretch improves lower body flexibility.

- Sit on a bed with one leg extended
- Loop a towel under the ball of the foot and pull gently.
- Hold for 15 seconds. Repeat 3 times on each leg.
Alternative: Stand facing a wall, placing your toes up the wall and heel down. Lean forward slightly to stretch the calf.
3. Chin Tuck
This exercise strengthens neck muscles and helps with posture.
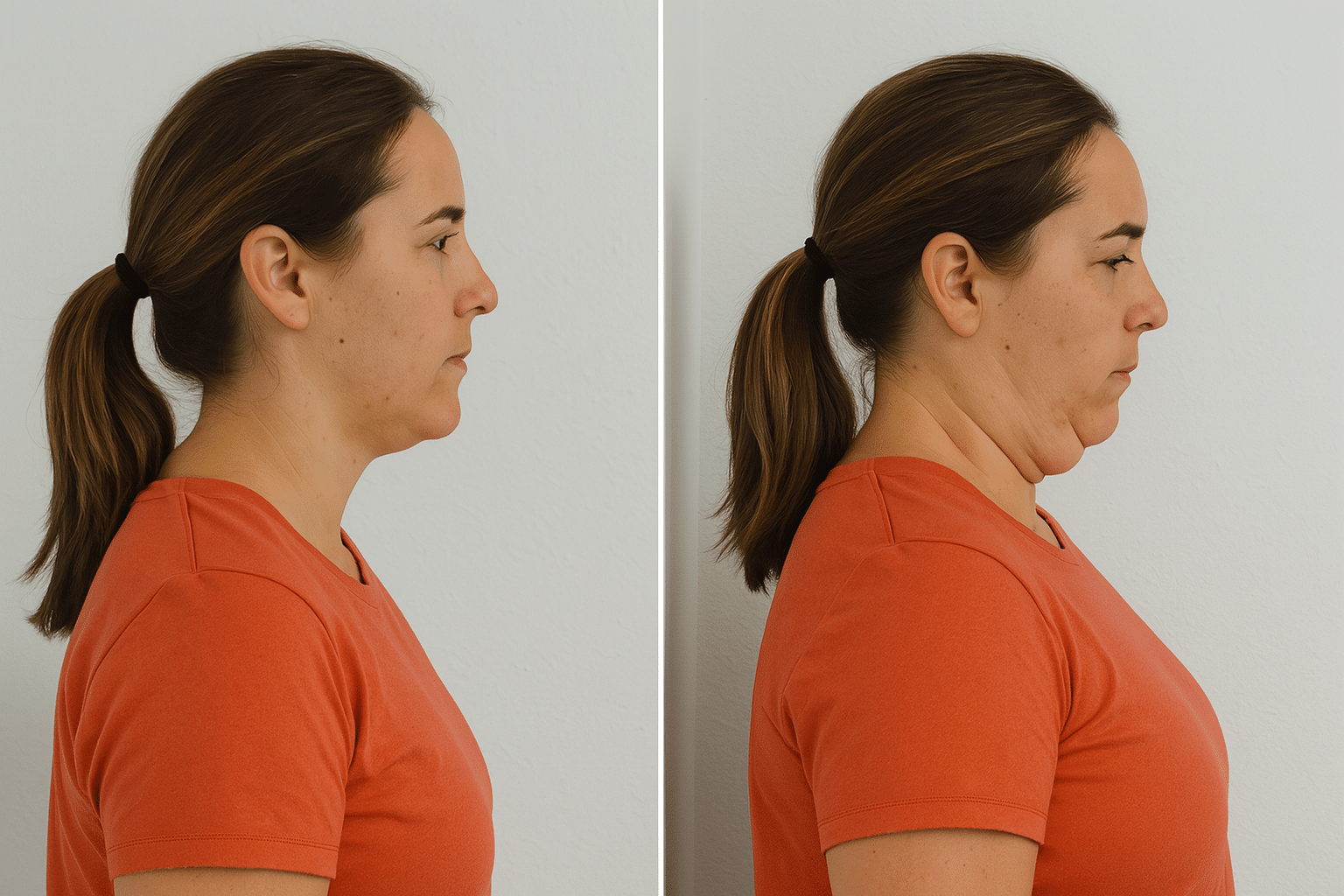
- Sit or stand with your neck in a neutral position.
- Gently tuck your chin backward, as though you’re trying to create a double chin. Imagine trying to squeeze a small object, like a piece of paper, under your chin without flexing your neck downward.
- Hold for 7 seconds. Repeat 5 times.
- For added resistance, press gently with your hands against the back of your head.
4. Scapular Retraction
This improves upper back strength and counters shoulder slumping.

- Sit or stand with a straight spine.
- Squeeze shoulder blades together as if holding a pencil between them.
- Hold for 7 seconds. Repeat 5 times.
5. Pelvic Bridge
Great for glutes and core strength—important for balance and walking.

- Lie on your back with knees bent, feet flat.
- Engage your core, then slowly press through your heels to lift your hips towards the ceiling. Activate your glutes as you lift, hold for 10 seconds.
- Repeat 10 times.
In addition to stretching, a complete exercise regimen for Parkinson’s should include:
- Aerobic Exercise: Walking, dancing, cycling, or high-intensity interval training can enhance brain health and cardiovascular fitness. Monitoring heart rate during aerobic and intense exercise is crucial for maximizing benefits and ensuring safety.
- Strength Training Exercises: Use resistance bands or bodyweight to maintain muscle strength.
- Tai Chi and Balance Exercises [2]: These improve stability and reduce fall risk.
- Deep Breathing and Meditation: Help manage stress and motor symptoms.
Work with physical therapists to develop a personalized exercise prescription. Physical therapists are experts in designing safe and effective exercise programs for Parkinson’s disease, focusing on balance, mobility, and fall prevention. A full functional evaluation can help tailor your new exercise program based on fitness level and current symptoms.
Understanding Parkinson’s Disease

Parkinson’s disease (PD) is a progressive neurodegenerative disorder that primarily affects movement and is classified under movement disorders. It is caused by the degeneration of dopamine-producing neurons in the brain—specifically in the substantia nigra.
The loss of these brain cells contributes to the motor symptoms and neurodegeneration seen in Parkinson’s disease. The loss of these dopamine-producing nerve cells disrupts the brain’s communication pathways, leading to motor symptoms such as tremors, stiffness, and slowed movement.
While the exact cause of the disease is still unclear, a combination of genetic factors, environmental exposures, and aging may contribute to its onset, particularly in the early stages. PD typically develops around age 60, though early-onset Parkinson’s can appear in younger adults.
Common Motor Symptoms of Parkinson’s Disease
Understanding the cardinal symptoms of PD can help guide your exercise program:
- Bradykinesia [3]: Slowness of movement that impacts coordination and daily living activities.
- Tremor: Often beginning in the hands or fingers, especially noticeable at rest.
- Rigidity: Muscle stiffness and resistance to movement in any part of the body.
- Postural Instability: A stooped posture and decreased balance, increasing the risk of falls.
- Other symptoms may include micrographia, slurred speech, depression, anxiety, and memory loss.
Why Parkinson’s Disease Exercises Matter
Regular physical activity and targeted Parkinson’s disease exercises can greatly improve motor skills, muscle strength, and cardiovascular fitness. Structured exercise programs and classes tailored for Parkinson’s patients not only boost mobility but also offer vital social support.
A balanced routine—combining stretching, balance work, resistance training, and aerobic activity—can help manage symptoms and may even slow disease progression.
According to the Parkinson’s Foundation, both moderate and high intensity exercise may have a neuroprotective effect, helping preserve dopamine-producing neurons and support long-term motor function.
Creating an Exercise Plan for Parkinson’s
Designing an effective exercise plan for Parkinson’s disease is all about creating a balanced, sustainable routine that addresses the unique challenges and symptoms each person faces.
Because Parkinson’s can affect motor skills, balance, and muscle strength in different ways, it’s important to work closely with a physical therapist who can help tailor an exercise program to your specific needs and fitness level.
Parkinson’s Disease Management at Home
Support your Parkinson’s disease management by incorporating:
- Nutrition: A balanced diet rich in protein, calcium, and fiber supports general well-being and is essential for managing parkinson’s.
- Relaxation: Meditation, yoga, or listening to calming music can reduce symptom severity.
- Massage Therapy: Helps reduce muscle rigidity and promote relaxation.
“Exercise is perhaps the most underutilized treatment for Parkinson’s disease. We now have strong evidence that regular physical activity — particularly aerobic and resistance training — not only improves motor symptoms, but may have neuroprotective effects that could potentially slow the progression of the disease.” –Dr. Michael Okun, MD – Medical Director, Parkinson’s Foundation; Professor of Neurology at the University of Florida
Final Thoughts
While there’s no cure for Parkinson’s yet, regular exercise plays a key role in maintaining independence, improving coordination, and slowing the neurodegenerative process. People with Parkinson’s who stay active often see improvements in both motor symptoms and overall well-being.
More research is underway—including PET scans and brain imaging—to better understand how exercise impacts dopamine levels and brain activity. Institutions like Yale School of Medicine are leading the way in studying exercise and neurodegeneration.
Not sure where to start? Talk to your doctor or a physical therapy specialist. A mix of intensity exercise, stretching, and balance training can significantly improve quality of life for people with Parkinson’s disease.
Staying active is one of the best long-term strategies for your body, brain, and future.
Get our trusted Master Guide to Vegetarianism (and the free recipes) and discover everything you need to know to succeed. Check out now!
Frequently Asked Questions
What are the best exercises for Parkinson’s disease?
The most effective exercises combine aerobic activity, strength training, balance exercises, and stretching. This includes walking, tai chi, resistance band work, and targeted Parkinson’s disease exercises like pelvic bridging or shoulder blade squeezes. Always focus on movements that improve motor function and help maintain independence.
Can exercise really slow the progression of Parkinson’s disease?
Yes. Research shows regular physical activity may have a neuroprotective effect, supporting brain health and potentially slowing the loss of dopamine-producing neurons. Both moderate intensity exercise and high intensity interval training (HIIT) have shown positive effects on motor symptoms and overall well-being.
How much exercise should someone with Parkinson’s do per week?
The Parkinson’s Foundation recommends:
- At least 150 minutes of moderate intensity exercise per week.
- Including strength training, stretching, and balance work at least 2–3 days per week.
- Your fitness level, stage of PD, and safety needs should guide your exercise prescription, ideally with support from a physical therapist.
Is it safe to start a new exercise program if I’m newly diagnosed?
Absolutely — and it’s highly encouraged. Starting in the early stages of Parkinson’s is key for maintaining motor skills, balance, and daily living abilities. Be sure to undergo a full functional evaluation and get clearance from your doctor or physical therapist before beginning any exercise regimen.