Do you often feel a sharp and electric shock-like pain on your buttock, radiating in the leg and sometimes into the foot? How about numbness or tingling sensations in your back and legs? Does it become more painful with standing, walking, or sitting? Then it might be a pain that is caused by a herniated disk. This article will help you understand herniated disc signs and symptoms.
What is a herniated disk?
A herniated disk is a condition of the Spine. It is a condition where one of the rubbery cushions of the vertebrates, called discs, tears or leaks through the wall, called annulus fibrosus, that encloses it. This can happen in other parts of the Spine. However, it is most common in the lumbar area or the lower back.
The Spine and What’s Inside It
Your Spine, also called the vertebral column or typically the backbone, is one of the essential parts of the body. It provides our body structure and support. It allows you to move and bend with ease. And it also protects the spinal cord.
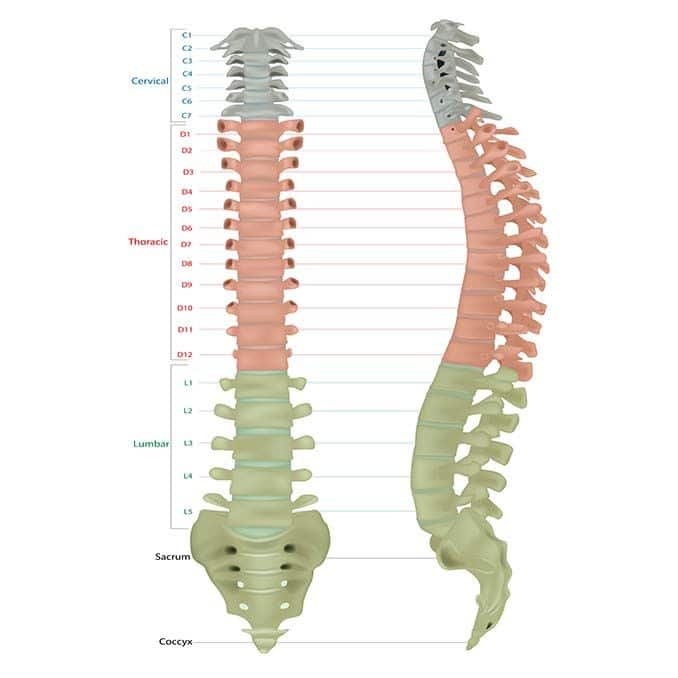
Your Spine stretches from the base of your skull to your tailbone and has five segments: cervical, thoracic, lumbar, sacrum, and coccyx. Together, it is made up of 33 vertebrates.
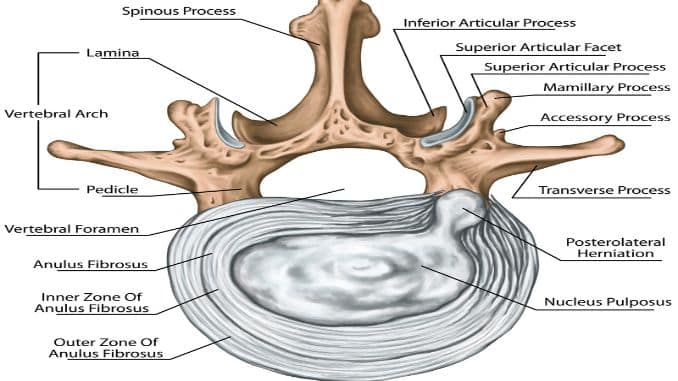
Inside each vertebra lies a disk stacked up between the vertebrae. They are composed of a soft, jelly-like center (called nucleus pulposus) enclosed in a tough and rubbery exterior (called annulus fibrosus).
It has three functions:
- Acts as shock absorbers of the Spine
- Acts as solid ligaments to hold the vertebrates of the Spine
- AIt acts as a cartilaginous joint to allow minimal movement of the Spine
A herniated disk happens when the nucleus pulposus pushes through the annulus fibrosus, creating a leak or tear in the disk. Factors like excessive weight, repetitive movements, and strain from sudden lifting or twisting of the back can also cause a herniated disk. It is often a result of aging-related wear and tears called disk degeneration.
Causes
There are several causes of disc herniation.
1. Wear and Tear on the Spine
Pain from a herniated disc is often the result of daily wear and tear on the Spine. This is also called degeneration.
Our backs carry and help distribute our weight, and those intervertebral discs are made to absorb shock from movement (such as walking, twisting, and bending). Because our discs work so hard to help us move so well, they can become worn out over time.
The annulus fibrosus (the tough outer layer of the disc) can start to weaken, allowing the nucleus pulposus (the jelly-like inner layer) to push through, creating a bulging or herniated disc.
2. Injury
An injury can also cause a herniated disc. For example, the sudden, jerking movements can put too much pressure on the disc, causing it to herniate. You can herniate a disc in a car accident.
Or you can herniate a disc by lifting a heavy object incorrectly or twisting significantly.
3. A Combination of Degeneration and Injury
It may be that an intervertebral disc has been weakened by wear and tear (degeneration), making it more prone to herniation should you experience a traumatic event.
Or it could be that your disc has become so weakened that something that doesn’t seem like a traumatic event can cause a herniated disc. This is the case when people herniate a disc sneezing (it does happen!). A sneeze doesn’t seem like a traumatic event that could lead to injury, but if you have an already-weakened disc, the sudden force of a sneeze can herniate a disc.
4. Tight Psoas
When you sit for extended periods, your psoas muscle may become tight. This, in turn, can pull your pelvis forward—which places pressure on your lumbar spinal discs. This additional pressure often results in lower back pain. And when the psoas is too tight, it can cause the disc to herniate.
Herniated Disc Signs & Symptoms
Sometimes, the protrusion can press or compress on a nerve which results in radiating pain to other parts of the body, numbness or tingling sensation, and muscle weakness.
- Sharp, burning, or radiating pain: If your lower back is affected, you will feel the pain in your buttocks or leg, particularly in the thigh, calf, or even foot, while if your upper back is affected, you will feel the pain on your arms or shoulders.
- Numbness or tingling sensation
- Muscle weakness
The herniated disc signs and symptoms may vary depending on where and what area is affected and if nerve compression is present.
Herniated Cervical Disk
- Presence of pain near or on your shoulder
- Presence of pain that radiates on your arms, sometimes hands, and fingers
- Neck pain increases upon movement (bending or turning the neck)
- Numbness or tingling sensation in your arms
Herniated Lumbar Disk
- Back pain.
- Numbness or tingling sensation in the legs or feet.
- Muscle weakness.
Diagnosis
Specific order tests can be done to diagnose and confirm herniated disk. Your healthcare provider will have to do an extensive examination. Some of these include:
- Magnetic resonance imaging (MRI): Most commonly used imaging test for a suspected herniated disk.
- X-rays: Helps rule out other causes of pain
- Computed tomography (CT): Can produce an image of the bones within the body.
- Myelogram: It involves an injection of a dye into your Spine using X-ray guidance for a CT scan which can reveal the location of the herniated disk.
- Electromyogram (EMG): Helps in determining what nerve it affects.
It also includes pain assessment, muscle reflex test, sensation, and muscle strength test.
Treatment
The initial goal of treatment is to relieve pain and other herniated disc signs and symptoms. The herniated disk will slowly improve for most who experience this condition from several days to weeks.
Medications
Your doctor may prescribe over-the-counter medications to address mild to moderate pain. This includes acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others), or naproxen sodium (Aleve).
Surgery
If conservative treatment fails to improve or relieve herniated disc signs and symptoms after six weeks, your doctor might recommend having surgery to remove the protruding portion of the disk.
Physical Therapy
Exercise programs made by a physical therapist could help in relieving the pain.
Corrective Exercises for Herniated Disc
Decreasing stress on the Spine is one of the main goals of treatment for herniated discs. Therefore, exercises that could improve core stability and posture, as well as those that correct muscle imbalances, can significantly help in doing this. Here are some of the exercises:
1. Hip Flexor Stretch
Kneel on a soft surface and bring one leg in front, placing the foot flat on the ground so the knee, positioned over the ankle, is bent at about a 90-degree angle. The back knee should remain on the cushioned surface and be bent at a 90-degree angle. Slide the front foot forward a few inches. Brace the abs and squeeze the glute of the side being stretched. Shift the hips forward. The back knee angle should now be slightly greater than 90 degrees. Hold for 10 seconds, perform 5-10 repetitions, then switch sides.
Try starting from a standing position for a version of the stretch that’s backward the knees. Take a big step backward with one leg. Bend the front knee until it’s over the front foot while simultaneously shifting the hips forward. Keep the back leg straight throughout. Hold for 10 seconds, perform 5-10 repetitions, then switch sides.
2. Hamstring Stretch
Stand next to a bench or table. Lift your leg onto the table so it is fully extended and straight. Rest your hands on the top of your upper leg for stability. Slowly lean forward, keeping your leg and back straight until you feel a stretch in your hamstring area. Hold the stretch for 10 seconds, then stand back up and rest. Perform 5-10 repetitions and switch sides.
3. Bilateral Knee to Chest
Lie on the floor, arms out to the side and knees bent. Slowly bring one knee toward the chest, then the other, aided by placing both hands on the back of the thighs. Hold for 10 seconds and perform 5-10 repetitions.
4. Single Knee to Chest
From the initial position for the Bilateral Knee to Chest, slowly bring one knee close to the chest, aided by pulling with both hands. Hold for 10 seconds and perform 5-10 repetitions. Switch sides.
5. Pelvic Tilts
Lay on your back with your arms by your sides, your knees bent, and your feet flat. There should be a space between the floor and your low back. Inhale first, and then initiate the pelvic tilt movement as you exhale. When you let your breath out, your belly button should come toward your Spine as you tilt the bottom of your pelvis up. This will result in your low back gently stretching and reaching in the direction of the floor. Inhale to come back to the starting position. Perform 10 repetitions.
6. Bridges
Lay on your back with your arms by your sides, your knees bent, and your feet flat. Make sure your feet are hip-width apart. Push through your heels to raise your hips, creating a straight line from your knees to your shoulders. Squeeze your glutes and brace your core. If your hips sag or drop, lower yourself back on the floor. The goal is to maintain a straight line from your shoulders to your knees and holds for 20-30 seconds. You should begin by holding the bridge position for five-second repetitions as you build your strength.
7. Iso Hip Flexion
Start in the same position as the Knee to Chest stretch. Draw both knees toward your chest until your thighs and torso form a 90-degree angle. Place your hands on your knees and try to move them closer to your wardrobe, but resist with your hands so no actual movement occurs. Hold for 10 seconds and then relax and perform 10 repetitions.
8. Safe Crunch
Lie on your back with your left leg extended. Your right knee should be bent and your right foot flat. Place your hand’s palms down on the floor underneath the natural arch in your lower back. Slowly raise your head and shoulders off the floor without bending your lower back or Spine, and hold this position for 5 seconds as you exhale. Perform 5-10 repetitions and then switch legs.
9. Bilateral Knee Raise
Sit on the edge of a chair or bench with your knees and feet together. Lean slightly backward, keeping shoulders pulled back and chest up. Bring your knees to your chest, then extend them back towards the ground. Perform 10 repetitions.
10. Air Bike (more advanced progression)
Sit on the edge of a chair or bench with your knees and feet together. Lean slightly backward, keeping shoulders pulled back and chest up. Bring your knees towards your chest, then perform a pedaling motion. Make sure you don’t simply push the feet in and out but form a circular motion with them. Perform 10 repetitions pedaling away from you and 10 repetitions pedaling toward you.
11. Accordions (most advanced progression)
Sit on the ground with your knees bent and feet flat. Your hands should be extended to the sides and parallel to the ground. Raise your feet off the ground and bring your knees toward your chest. At the same time, get your hands toward one another and exhale, pretending you are squeezing an accordion. Then extend your legs straight and parallel to the ground and your arms out to the sides.
Unlock your hip flexors program for Herniated Disc
Introducing the Unlock Your Hip Flexors Program (UYHF), a practical, easy-to-follow program you can use today for Herniated Disk.
Why UYHF?
- Since tight psoas muscle can pull your pelvis forward—which places pressure on your lumbar spinal discs that could cause the disc to herniate, the UYHF could help loosen this muscle to correct this process.
- Contains strengthening exercises for the core and the muscles that support your back to improve posture. Prolonged sitting and no physical activity can weaken these muscles. A substantial body can help support and stabilize your Spine, thus avoiding pain and injury.
Takeaway
Fortunately, conservative treatments can relieve pain and other herniated disc signs and symptoms for at least four to six weeks. It usually improves over time. However, leaving it as is will make it worse. It may result in chronic pain and loss of motor and sensory control of the affected area. It is always best to consult with a doctor for a more suitable approach to treating it.