Stroke is one of the most common medical conditions affecting people worldwide. According to the 2020 Fact Sheet of the World Health Organization, stroke remains the second leading cause of death and disability globally with over 13 million people experiencing a stroke each year and around 5.5 million people dying from this condition. According to the Center for Disease Control and Prevention, in the United States alone, stroke became the fourth leading cause of death, accounting for 795,000 deaths each year.
With the prevalence of stroke and how rampant its effects, access to information about this condition is important. Resources regarding how to prevent this condition and improve recovery are vital for saving lives and improving the quality of life of those affected.

What is Stroke?
Stroke, also known as cerebrovascular accident (CVA), happens when there’s a sudden loss of neurological function due to loss of blood flow to the brain. Loss of blood flow can cause inefficiency in the function and death of the brain cells. Consequently, brain cell death can cause lasting brain damage, long-term disability, or even death.
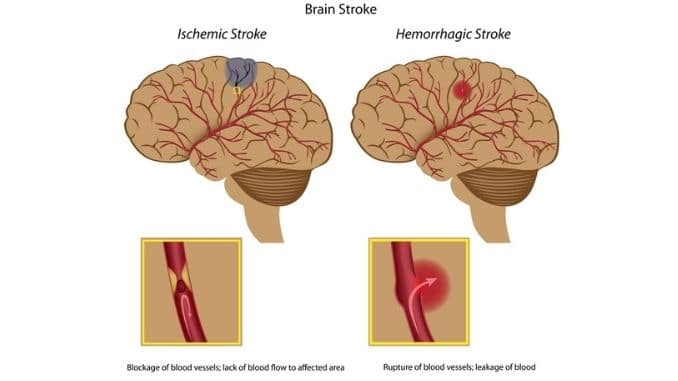
Stroke has three main types, exhibiting different causes: Ischemic Stroke This is the most common type, with 80% of individuals with stroke affected. This results from a blockage of a blood vessel caused by a plaque or clot, harming blood flow. These clots are build-up from the blood vessels. The most common sites for lesions to occur are at the neck (common carotid artery), at the brain (middle cerebral artery), and at the junction of the vertebral arteries with the basilar artery. Hemorrhagic Stroke This type of stroke occurs when there’s a rupture of the blood vessels, causing leakage of the blood in or around the brain. This leakage increases pressure on the skull, causing injury to brain tissues and restriction of blood flow. High blood pressure, aneurysm, or arteriovenous malformation can cause the blood vessels to rupture, contributing to hemorrhagic stroke. Transient Ischemic Attack (TIA) Another type of stroke is a transient ischemic attack (TIA). It’s sometimes called a mini-stroke because the interruption of blood supply is temporary. The damage to the brain cells isn’t permanent, and the symptoms of the deficit may last for only a few minutes or several hours, but do not last longer than 24 hours. Even if the TIA is temporary, a person is still at a much higher risk of having a stroke after TIA.
Risk Factors for Stroke
Non-Modifiable Risk Factors
Age: This is the single most important factor worldwide. After 55 years of age, the incidence is raised for both males and females. Also, the risk doubles after this age. Gender: Males are more affected than females, although many risk factors are specific to women. Women with early menopause have twice the risk of developing ischemic stroke compared to women with later menopause. The use of estrogen alone or estrogen plus progestin increases the risk of ischemic stroke. Race: According to the Centers for Disease Control and Prevention (CDC), the risk of having a first stroke is nearly twice as high for African Americans compared to Caucasians. Caucasians are still at high risk in comparison with Asians. The CDC added that African Americans have the highest rate of death due to stroke. Family History: Genetics can also increase your risk factors for having a stroke. Having a family history of stroke or TIA can predispose a person to develop the same condition. Although recent studies have shown that genes can create an overlap between modifiable and non-modifiable factors, genetic risk factors are increasingly recognized as potentially modifiable, either directly or through the transformation of gene-environment interactions.
Modifiable Risk Factors
Major modifiable risk factors for developing a stroke are hypertension, heart disease, the condition of the heart rhythm, and diabetes mellitus.
Hypertension:
This is the most important modifiable risk factor for both ischemic and hemorrhagic stroke. In fact, hypertension can increase the risk of stroke by sevenfold. Sufficient evidence supports public health efforts aimed at reducing the prevalence of poorly controlled blood pressure, thereby decreasing the risk of stroke and other conditions associated with it.
Incidence of Transient Ischemic Attack:
TIA is associated with common carotid artery disease and is an important sign of stroke risk. This can help in determining common carotid artery disease, which will help in lowering stroke incidence.
Heart Disease:
Heart conditions such as congestive heart failure and coronary artery disease can increase the occurrence of stroke twofold.
Diabetes Mellitus:
People with diabetes are susceptible to hypertension and heart disease, which can predispose them to develop stroke. Nevertheless, diabetes alone can still double the risk of having a stroke.
Cigarette Smoking:
Cigarette smoking can increase the buildup of plaque, can damage the blood vessels, and can contribute to raised blood pressure.
Alcohol Consumption:
According to studies, the consumption of alcohol and stroke depends on the stroke type. Heavy drinking is associated with a raised risk of ischemic stroke, whereas binge drinking can increase the risk of hemorrhagic stroke. Although, light-to-moderate alcohol consumption comprising up to 2 drinks per day in men and up to one drink for women can be defensive against stroke.
Elevated Cholesterol Level:
People with high Low-Density Lipoprotein (“Bad Cholesterol”) compared with High-Density Lipoprotein (“Good Cholesterol”) raised a predisposition to stroke. A raised cholesterol level contributes to raised plaque buildup in the blood vessels.
Obesity:
Obesity indirectly increases the risk of having a stroke, as it is correlated to risk factors such as hypertension and diabetes.
Lifestyle:
The level of physical activity and diet plays a role in developing stroke. Firstly, diet influences the risk of having a stroke, as a poor diet predisposes a person to other risk factors such as hypertension, raised cholesterol levels, and diabetes. Furthermore, a sedentary lifestyle also plays a role in developing these other risk factors.
Signs, Symptoms, and Complications of Stroke
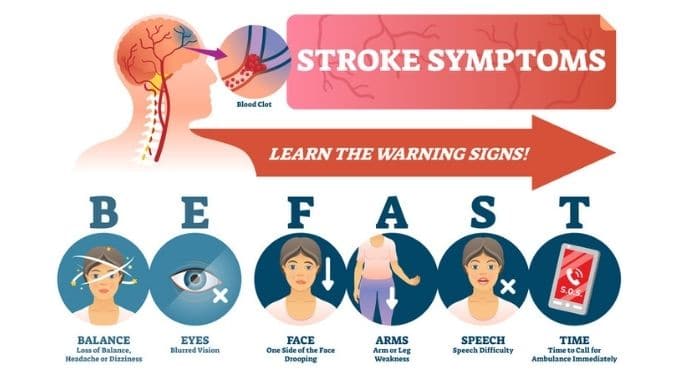
According to the American Heart Association, the following are the early warning signs of stroke:
- Sudden numbness or weakness of the face, arm, and leg, especially on one side of the body
- Sudden confusion, trouble speaking, or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance
- Sudden severe headache with no known cause.
If you spot these early signs, call an ambulance right away.
Depending on the area of the brain affected, the severity, and extent of the tissues damaged, a range of problems can arise after a stroke. These complications can be long-term, as this condition can cause lasting damage to the brain tissues, resulting in long-term disability. The following complications can develop after a stroke:
- Altered consciousness
- Speech and language disorders
- Inability or difficulty swallowing
- Cognitive dysfunction
- Altered emotions and changes in behavior
- Muscle weakness
- Poor motor control
- Loss of balance
- Impaired sensation
- Dysfunction of skilled movements
Other complications such as:
- Cardiovascular dysfunction
- Pulmonary dysfunction
- Clot formation in veins (called deep vein thrombosis), and embolus formation on the pulmonary system because of immobilization
- Fractures and osteoporosis
Area of the Body Affected by Stroke
The area of the body affected by stroke is opposite to the side of the brain affected. For example, if the left side of the brain is affected, its signs and symptoms will display on the right side of the body.
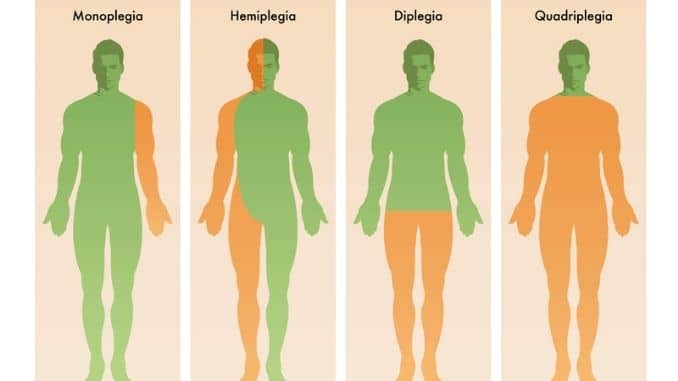
Types of Paralysis in Stroke
There are different types of paralysis, depending on the area of the impairments:
- Monoplegia: This paralysis manifests in one leg or arm
- Paraplegia: This paralysis affects both legs
- Hemiplegia: This affects one leg and arm on the same side of the body
- Tetraplegia: This paralysis affected both legs and arms
Use this image – but crop the top of the image to remove the text that reads ‘Types of Cerebral Palsy’
Most of the time, the area of paralysis can give healthcare providers a general overview of possible areas of the brain affected.
Another way of determining the type of paralysis is by how the muscles act:
- Flaccid Paralysis: Flaccidity is a type of paralysis that refers to a complete lack of muscle movement with muscles losing their mass and bulk.
- Spastic Paralysis: Meanwhile, spastic paralysis involves tightening and hardening of the muscles upon movement.
Diagnosing Stroke
Tests and procedures are done to rule out any conditions demonstrating similar signs and symptoms. Healthcare providers will order imaging tests to look at the blood vessels of the brain. These procedures determine what type of stroke and the area of the brain is affected. The rule of thumb is, knowing the stroke early will allow doctors to treat the condition quickly and prevent more debilitating outcomes.
The following are the tests conducted to diagnose stroke:
- Computed Tomography (CT scan) of the brain
- Magnetic Resonance Imaging (MRI) of the brain
- Other tests, such as Doppler ultrasound or angiography for the blood vessels
- Blood Tests and heart tests such as an electrocardiogram (EKG)
Additionally, an examination will help identify and monitor impairments. The risk factors for stroke are assessed for subjective assessments. Meanwhile, a physical examination involves checking for signs and symptoms.
Your doctor will assess for the following:
- Confusion
- Coordination and balance
- Mental alertness
- Numbness or weakness in your face, arms, and legs
- Trouble speaking or seeing clearly
The Different Stages of Stroke
Just like other conditions, stroke undergoes different stages of recovery. Many stroke survivors will wonder how long they will need to recover, or if they will ever get back to their previous norms. Therefore, identifying the course of the recovery helps in developing approaches to regaining controlled movement and function after a stroke.
There are seven recognized stages of stroke recovery. Each stage is honed into what is known as the Brunnstrom Approach. This framework will utilize patterns of movement at each stage as part of the process and use them to aid in rehabilitation.
Stage 1: Flaccidity
This stage happens immediately after stroke, where flaccidity occurs. Flaccidity is a type of paralysis that refers to a complete lack of muscle movement with muscles losing mass. Due to this paralysis, the person with a stroke cannot initiate any muscle movements on the affected side of their body. In addition, there is a lack of or decreased reflexes on the affected side. Without early intervention or physical therapy, the unused muscles become much weaker and begin to atrophy.
To prevent more weakness and loss of muscle mass, unused limbs still need stimulation to maintain or form connections to neurons. Though the nerves and connections that originally controlled your affected limbs may be damaged too much to create voluntary movements, it is still possible to regain movement in later stages of recovery.
Stage 2: Spasticity begins to develop
The second stage highlights the beginning of spasticity or increased tone and stiffness of the muscles. The muscles begin to make incremental changes in muscle tone, plus abnormal involuntary movements. Spasticity is a type of paralysis that is velocity-dependent, meaning the stiffness will appear as moving the limb faster. This stiffness will create resistance to any passive movements.
In addition, a synergistic movement may start to appear at this stage. Synergy means that trying to make one movement on the affected side ends up making multiple movements. Some of the components of the synergies may begin to appear at this stage, emerging common patterns of movement that may limit the person’s muscles to specific movements.
Stage 3: Spasticity reaches its peak
Stage 3 is when severe spasticity occurs. Increased resistance to movement caused by muscle stiffness and increased tone will interfere more with movement or will cause more discomfort or pain. At this stage, spasticity is evident through the full range of motion. Furthermore, a person at this stage can initiate minimal voluntary movement along with the synergistic pattern but still is unable to control the form of the resulting movement.
In this stage, the muscles with severe spasticity are likely to be more limited in their ability to move and may require help to do this. Patients and family/caregivers should be educated about the importance of maintaining range of motion and doing daily exercises. It is important to minimize spasticity triggers in training.
Stage 4: Spasticity begins to decline
During this stage, patients will still demonstrate initial voluntary movement within the synergistic pattern, but then will be able to move out of it. In addition, the spastic movement begins to decline, allowing more range of movement because of less resistance. In this stage, the movement combinations that do not follow the paths of basic limb synergies are mastered first with difficulty, then with increasing ease.
Now that some degree of movement control is allowed, the focus during this stage is to build strength, continue with improving range of motion, and improve muscle control.
Stage 5: Typical movement combination of stroke loses its dominance
In this stage, spasticity begins to decrease, and the synergy patterns decline. The patient can initiate movement despite some presence of the patterns, allowing more coordination. In this stage, more difficult movements are mastered, and the basic synergies lose their dominance.
Stage 6: Individual joint movement becomes possible
At stage six, spasticity completely disappears. The patient becomes capable of the full spectrum of movement patterns. Individual joint movements are now possible, and synergy patterns become much more coordinated. Despite the movement patterns in near normal, there’s still difficulty completing complex and difficult rapid tasks. The overall coordination still approaches normalcy.
Stage 7: Restored normal function
The last stage in Brunnstrom’s Approach is when the patient regains full function in the areas affected by the stroke. They are now able to move their arms, legs, hands, and feet in a controlled and voluntary manner.
Since there is full control over the muscle movements, synergy patterns have also returned to normal. Reaching stage seven is the ultimate goal for stroke rehabilitation.
This useful overview about the stroke, its nature, and stages, can help you better understand the causes of stroke, both modifiable and unmodifiable. More importantly, we have shared early symptoms that require immediate medical attention. For more information on navigating stroke recovery and rehabilitation, look for the second part of this article in the stroke series.
Your blood pressure is directly related to your risk of Stroke, so there is no better time to lower your blood pressure safely and naturally. Click here to learn how.