Osgood-Schlatters Disease (OSD) is an uncommon condition that involves inflammation and spurs in the growth plate of long bones. The disease usually affects adolescent males who play sports such as soccer, rugby, basketball, or other activities that involve frequent bending and squatting. OSD can be difficult to diagnose, but early recognition and treatment can reduce the potential for serious complications. Keep reading to learn more about this condition, its symptoms, risk factors, and how to treat it.
This morning I was working on this OSD article for you.
The idea came from an interview I had heard a few weeks back.
The interview was with Ryan Kesler, an ice hockey player for the Vancouver Canucks.
Since my ice hockey team is the Vancouver Canucks, I have seen him become an outstanding ice hockey player in the last few years.
He almost did not make it to the National Hockey League (NHL) because he had an injury that could have ended it all when he was a kid.
He had OSD, and if it was not for his father and his internal push to overcome his injury, his career in the NHL might never have happened.
His mindset of being determined, putting in hard work, and maintaining a never-give-up attitude to overcome his injury, in addition to a good rehabilitation program for exercise, helped him overcome his OSD.
Let’s chat about OSD and an Exercise Program for it.
What Is Osgood-Schlatters Disease (OSD)?
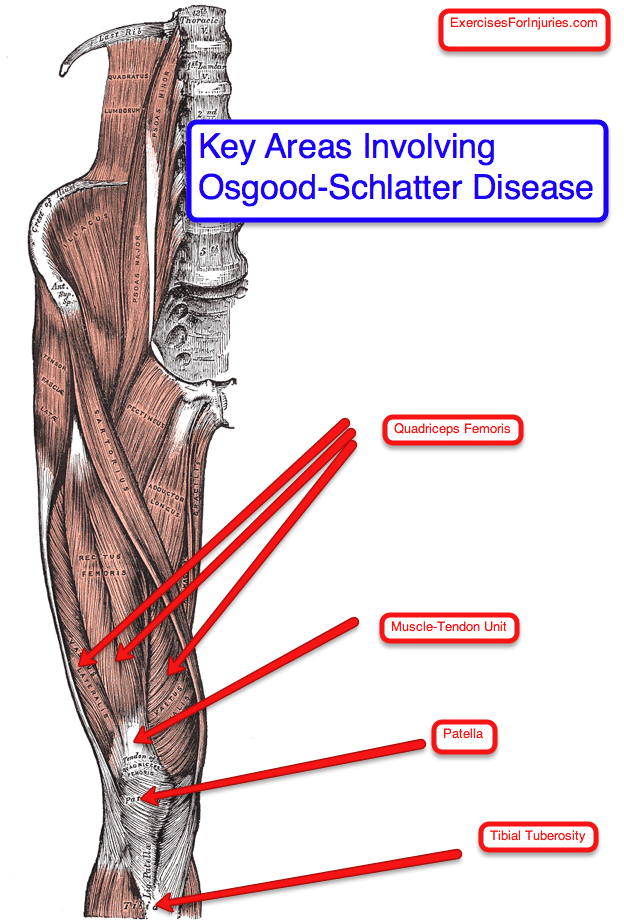
Osgood-Schlatters Disease is a condition found in active adolescents undergoing a growth spurt with pain and tenderness at the patella tendon, which connects with the lower leg. There ends up being traction (stress) of the muscle-tendon unit at tibial tuberosity, which leads to pain.
Symptoms of the condition come and go and can take months to years to resolve fully.
About 90% of people overcome the injury with rest, ice, activity modification, and exercise rehabilitation. Often it resolves after the closure of the tibial growth plate.
Other Names for OSD
- Tibial Apophysitis.
- Morbus Osgood-Schlatter
- Rugby knee
It is classified as a knee extensor problem (knee straightening out).
Often medical professionals will classify OSD as anterior knee pain.
Other injuries that fall into the anterior knee pain classification are:
- Patellar subluxation or dislocation
- Patellofemoral pain syndrome
- Jumper’s knee
The physical signs of Osgood-Schlatters are tenderness, warmth, or swelling at the tibial tuberosity.
Key Structures Involved in OSD
Who Gets OSD?
It is most often seen in teenage boys and young men. The age range in boys is 12 to 15, and if it is seen in girls, their age range tends to be 8 or 12 years. It is often seen after the boy or girl has had a growth spurt, and the symptoms gradually come on.
New research has shown that athletes with limited dorsiflexion could be at significant risk for OSD. It is thought that a decrease in dorsiflexion in the ankle leads to compensation in the leg with increased knee flexion, tibial inversion, and foot pronation during the stance phase of running. These three compensations may lead to more significant stress placed on the patellar tendon, leading to OSD.
What Can Cause OSD?
- Rapid growth and physical activity
- Athletes with poor ankle dorsiflexion
What Makes OSD Worse?
- squatting
- running
- walking up or down stairs
- cycling
- forceful contractions of the quadriceps muscle
- jumping (basketball, volleyball)
- kneeling
- hurdling
- repetitive hard landings place
- anything that puts excessive stress on the insertion of the patellar tendon
How is OSD Diagnosed?
- Physical exam by a qualified health care professional
- x-ray
- Ultrasonography or MRI will show changes in the distal part of the patellar tendon at the tibial tuberosity.
What can You Do to Overcome OSD?
- Modify activities
- Ice
- Decrease inflammation with over-the-counter or prescribed medication
- Infrapatellar strap
- Stretching
- Strengthening
- Often resolves after a growth spurt is done
- 10% to 12% of patients may need surgery
In one study (Kujala 1985), athletes had, on average, 3.2 months of training and 7.3 months of some activity modifications.
OSD Exercise Rehabilitation Program
Now let’s head into an exercise program that can help.
Stretching for OSD
- Prone quadriceps stretching
- Hamstring stretching
- Calf stretching
- Soleus stretching
Strengthening Exercises for OSD
- Single leg raises
- Prone hip extension
- Side-lying clam exercise
Mobility for OSD
- Ankle mobilization
Where to Get More Information on OSD
I understand that you might wish to study the subject further. Here are the resources I used to write the article. I hope you enjoyed it. It was a pleasure to create. Please let me know if you would like me to write more in the future. Take care.
Rick Kaselj, MS